CHICAGO – Subtle differences in brain anatomy among older individuals with normal cognitive skills may be able to predict both the risk of developing Alzheimer’s disease in the following decade and how quickly symptoms of dementia would develop. In their analysis of magnetic resonance (MR) images from two separate study groups, researchers from Rush University Medical Center and Massachusetts General Hospital (MGH) found that, among individuals in whom specific brain structures were thinnest, the risk of developing Alzheimer’s was three times greater than in those with above-average thickness. The study appears in April 13 issue of Neurology.
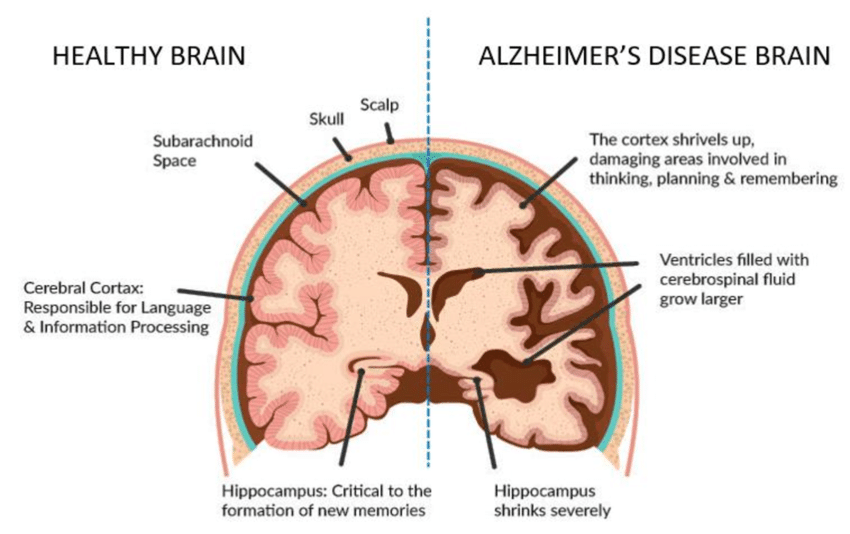
“We know, primarily from postmortem studies, that changes characteristic of Alzheimer’s disease can be present in the brains of cognitively normal people,” says Dr. Brad Dickerson, of the MGH department of neurology, lead author of the paper. “But since it takes a long time to follow people through initial symptom development to eventual diagnosis, how that process occurs has received very little study. We used what we know about the signature brain changes seen in patients with Alzheimer’s dementia, measured those areas in individuals with no symptoms and eventually determined that those who ultimately developed dementia showed subtle shrinking long before they had any symptoms.”
“The MR measurements could be very important indicators to help identify who may be at risk of developing Alzheimer’s dementia. If a drug therapy or treatment is developed in the future, those who are still without symptoms but at great risk would benefit the most from treatment,” said Leyla deToledo-Morrell, PhD, senior author of the paper and professor in the department of neurological sciences at Rush University Medical Center.
Participants in this study, men and women in their 70s with similar levels of education, were enrolled in two long-term research investigations of brain changes in older individuals, one based at Rush and the other at MGH. Upon entering the studies, participants had a comprehensive clinical examination, neuropsychological evaluation including memory testing, and brain MR imaging. At annual follow-up visits, each was reassessed to determine whether they were cognitively normal or if they had mild cognitive impairment or probable Alzheimer’s dementia.
The Neurology study analyzed data from participants who were cognitively normal at the outset and had at least four follow-up visits – a group that totaled 50 participants who remained cognitively normal at the end of the study period, and 15 who had developed Alzheimer’s over an average time span of about nine years. In both study groups, the baseline MR images revealed that areas of the cerebral cortex associated with Alzheimer’s in previous studies tended to be thinner in participants who went on to develop dementia.
Among those in whom these signature brain areas were the thinnest, 55 percent developed dementia during the study period, compared with 20 percent of those with average cortical thickness and none of those in whom cortical thickness was above average. Participants with the thinnest cortical areas also developed Alzheimer’s significantly faster than those with average thickness.
“Comparing the data from the Chicago and Boston sites showed very similar results,” said deToledo-Morrell. “Pulling together the data from both sites makes the findings that much stronger.”
Adds Dickerson, who is an associate professor of Neurology at Harvard Medical School, “We believe these MR measurements can be powerful markers of the pattern of brain atrophy in Alzheimer’s disease and are investigating their use in several ways, including assessing dementia risk in asymptomatic individuals. Our current results are preliminary and are not ready to be applied outside of research studies, but we are optimistic that this marker will be useful in guiding clinical care in the future.”
Additional co-authors of the Neurology study – which was supported by grants from the National Institute on Aging and the Alzheimer’s Association – are Travis Stoub, PhD, and Dr. Raj Shah, Rush University Medical Center; Dr. Bradley Hyman and Dr. Deborah Blacker, MGH; Dr. Reisa Sperling, Brigham and Women’s Hospital; Ronald Killiany, PhD, Boston University School of Medicine; and Marilyn Albert, PhD, Johns Hopkins School of Medicine.
About Rush University Medical Center
Rush University Medical Center, Chicago, is an academic medical center that includes a 676-bed hospital serving adults and children. Rush University includes Rush Medical College, the College of Nursing, College of Health Sciences and the Graduate College. Rush is a thriving center for basic and clinical research, with physicians and scientists involved in hundreds of research projects developing and testing the effectiveness and safety of new therapies and medical devices.
About Massachusetts General Hospital
Massachusetts General Hospital conducts the largest hospital-based research program in the United States, with an annual research budget of nearly $700 million and major research centers in AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, reproductive biology, regenerative medicine, reproductive biology, systems biology, transplantation biology and photomedicine.

0 Comments